An Assessment of Public Understanding of Antibiotic Resistance and Misuse
Josiah NelsonTyler Burslie
North Dakota State University
Abstract
In the early years of their use, antibiotics were seen as “miracle drugs.” However, in the time since their discovery the miracle has faded into an evolutionary arms race between scientists and doctors developing new antibiotics and their bacteria foes. Much of the source of the problem lies with the improper use of antibiotics. Ignorance of antibiotic resistance is at least partially to blame for misuse. A random survey of 30 people was conducted to provide an assessment of the general public’s knowledge of antibiotics and antibiotic misuse. The results of this study aid in increasing awareness of antibiotic misuse and resistance.
Introduction
After the discovery of penicillin in 1928, antibiotics became widely produced and distributed. Back then there wasn't a warning label attached saying, “if mishandled, will cause bacteria to become resistant to antibiotics.” Unfortunately, misuse of these drugs has led to antibiotic resistance, rendering the drugs ineffective. Dr. Stuart Levy discusses the significance of the problem saying, “Resistance originates as a local phenomenon but can expand to global proportions” (Levy, 2001).
Antibiotic resistance today is a result of increased production, distribution, and use of antibiotics. The increased exposure of bacteria to antibiotics has led to the creation of multiple resistant bacteria by the accumulation of genetic resistance determinants. This multiple resistance has led to therapy being unsuccessful even against common organisms such as E. coli and Staphylococcus. Some species that are resistant to newer drugs are emerging at an increased rate probably due to environments already contaminated with antibiotics. Newer drugs meant to fight this resistance can cause problems of their own, sometimes producing side effects that limit their use and may cause tissue damage, such as with the drugs Levaquin and Ciprofloxacin (Cipro Tendonitis). Failure to stop the spread of antibiotic resistance compromises the health of our community. Increasing numbers of multiply-resistant pathogens are appearing in hospitals and outpatient clinics. This problem was traditionally only seen in large city hospitals (Levy, 1983). This is a problem that needs to be addressed more publicly so that steps may be taken to curb the spread of antibiotic resistance.
In 1998, approximately 50 million pounds of antibiotics were produced in the United States alone. About half of this was used in hospitals and homes, most of the rest being used for treating animals (Levy, 2001). “Although the antibiotic agent is an important factor impacting antibiotic resistance, its selective role relates not only to the total amount, but how it is being used. The same antibiotic provided in different ways can have significantly different effects on antibiotic resistance” (Levy, 2001). Observers have documented antibiotic misuse with cases of physician-written prescriptions for diagnoses that lacked appropriate suspicion of bacterial infection, including a study that used a medical student with a simulated illness. Another study surveying antibiotic usage in hospitals in Pennsylvania found that in surgical prophylaxis, 20 to 25 percent of antibiotic misuse was unnecessary (Levy, 1983). Antibiotic resistance can also be linked to household antibacterial products.
There are over 300 nonprescription products on the market today that contain antibacterial agents. This widespread overuse of antibiotic chemicals has contributed to increased antibiotic resistance (Levy, 2001). The initial problem of resistance has continued to snowball into more serious issues. As Stuart Levy explains, “Alongside the widely recognized multiply-resistant enteric organisms have now appeared new strains of enterococci which are resistant to all antibiotics currently available, even the most recently developed cephalosporins. While there is general recognition among medical personnel that the problem of antibiotic resistance exists, there is also apathy and/or hopelessness in changing the situation” (Levy, 1983). But with increased awareness and education, we may be able to fight antibiotic resistance.
The purpose of this study was to provide a baseline of information on the general public's awareness of antibiotic resistance and proper use of antibiotics. This information can then be contributed to educational resources to help raise awareness and understanding of antibiotic resistance. As Levy says, “It is only by raising concern at the level of all individuals that this over-utilization of antibiotics can be eliminated and the re-establishment of an environment low in resistance genes can be realized” (Levy, 1983). Education and awareness are pivotal to reaching solutions in the fight against resistance.
Materials and Methods
This survey was conducted by surveying a sample of North Dakota State University students and faculty on campus. Participants were given a simple questionnaire to fill out (See Appendix A). The survey was completely voluntary and anonymous to protect the privacy of those surveyed. A total of 31 people were surveyed and their answers were compiled and assessed.
Results
In this section of our report, we present the results of our survey, displaying the questions and answers in the same order in which they appear on our survey form.
- Ages of men surveyed-46, 37, 36, 29, 24, 21, 20, 19, 19, 26, 24, 25, 32, 23, 23, 20, 21, 22
Ages of women surveyed-33, 30, 26, 26, 24, 22, 23, 24, 22, 30, 21, 26, 22 - A total of 18 men and 13 women were surveyed.
- Are you familiar with the concept of antibiotic resistance? Of the men surveyed 13 of 18(72%) answered yes. Of the women, 9 of 13(69%) answered yes.
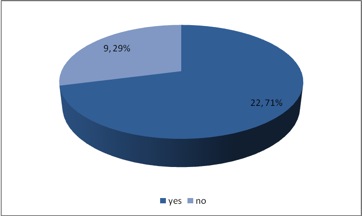
Figure 1: Familiary with antibiotic resistance. Figure 1 displays total answers given for question 3 of the survey, “Are you familiar with the concept of antibiotic resistance?” - Have you ever been prescribed an antibiotic? 11(61%) of 18 men answered yes, with 4 saying they are unsure. Of the women surveyed, 11(84%) answered yes with one answering no and one answering unsure.
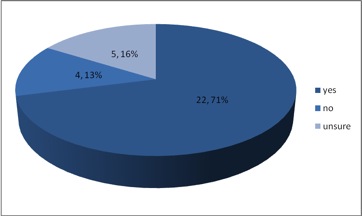
Figure 2: Antibiotic Perscription. Figure 2 displays total answers for question 4 of the survey, “Have you ever been prescribed an antibiotic?” - If yes to question, did you use the drug for the full extent of the prescription? Of the men who answered this question, 8(57%) of 14 said no, while 7(63%) of 11 women answered yes.
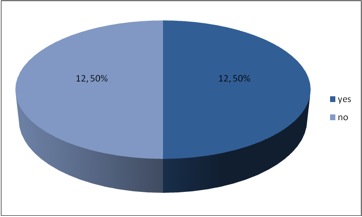
Figure 3: Rate of completing full dose prescribed. Figure 3 displays total answers for question 5 of the survey, “did you use the drug (antibiotic) for the full extent of the prescription?” - Have you ever asked a doctor to prescribe an antibiotic for common cold or flu symptoms? Of the men surveyed, 15(83%) of 18 answered no, while 9(69%) of 13 women also said no.
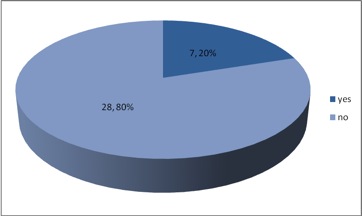
Figure 4: Requesting Antibiotics Behavior. Figure 4 displays total answers for question 6 of the survey, "Have you ever asked a doctor to prescribe an antibiotic for common cold or flu symptoms?” - Do you regularly use antibacterial soap or other cleaning products with antibacterial agents in your home? Most of the men surveyed, 10(55%) of 18, answered yes to the question, with the remainder being equally divided in their answers. 10(76%) of 13 women also answered yes, while 2 answered no and one was unsure.
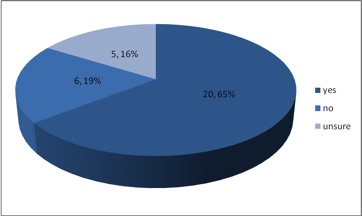
Figure 5: Use of antibacterial household products. Figure 5 displays total answers for question 7 of the survey, "Do you regularly use antibacterial soap or other cleaning products with antibacterial agents in your home?” - Would you be interested in learning about antibiotics and antibiotic resistance? Only 3(16%) of 18 men answered yes. 9 answered no while 6 answered maybe. Of women surveyed, only 4(30%) of 13 answered yes. 7 answered no while 2 answered maybe.
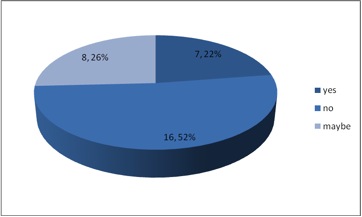
Figure 6: Interest in learning more about antibiotic resistance. Figure 6 displays total answers for question 8 of the survey, “Would you be interested in learning about antibiotics and antibiotic resistance?”
The results of this survey show both positive and negative results in relationship to the general public's knowledge of antibiotic resistance. It’s pleasing to see that of those surveyed, 72 percent of men and 69 percent of women are familiar with the concept of antibiotic resistance. This finding is important because it shows that the majority of those surveyed have some level of awareness of the issue. Also, 83 percent of men and 69 percent of women said they’d never asked a doctor to prescribe an antibiotic just for cold or flu symptoms. This is another positive result of this study because it shows that most people are trusting in the diagnosis of their doctors and are not trying to self medicate with antibiotics.
Unfortunately not all results are this positive. Some 57 percent of men surveyed said they did not use an antibiotic for the full extent of their prescription which increases the risk that the drugs will not work to their full effect. Failure to complete the course of treatment provides the conditions attributable to propagating resistance. However, 69 percent of women said they properly carry out their prescription. Most surveyed use antibacterial soap or cleaning products in their homes which can be a promoter of antibiotic resistance. The most disheartening result of the survey is that there seems to be a lack of interest in the issue with only 16 percent of men and 30 percent of women being interested in learning about antibiotics and resistance.
To curb the spread of antibiotic resistance there must be public concern for the issue at a local and global level. By slowing antibiotic misuse, we may see a reduction in resistance. Less money would need to be spent on the development of newer drugs and it could be possible that some older antibiotics may become more effective. The solution to the problem of antibiotic resistance starts with education. Hopefully this study will help progression towards a greater public understanding and awareness of antibiotic resistance and misuse.
Works Cited
Cipro Tendonitis and Levaquin Tendonitis are BAD News… (n.d.) Retrieved December 6, 2010, from http://www.side-effects-site.com/cipro-tendonitis.html
Levy, Stuart B. "Antibiotic Resistance: Consequences of Inaction." Clinical Infectious Diseases 33.3 (2001): S124-129. Print.
Levy, Stuart B. "Antibiotic Resistance." Infection Control 4.4 (1983): 195-97. Print.
Appendix A: Survey Questionnaire 1. Age ____ 2. Gender M / F 3. Are you familiar with the concept of antibiotic resistance? (Circle One) Yes / No 4. Have you ever been prescribed an antibiotic? (Circle One) Yes / No / Unsure 5. If yes to question, did you use the drug for the full extent of the prescription? (Circle One) Yes / No 6. Have you ever asked a doctor to prescribe an antibiotic for common cold or flu symptoms? (Circle One) Yes / No 7. Do you regularly use antibacterial soap or other cleaning products with antibacterial agents in your home? (Circle One) Yes / No / Unsure 8. Would you be interested in learning about antibiotics and antibiotic resistance? (Circle One) Yes / No / Maybe Thank you for completing this survey.
If you would like to see previous comments or leave comments about this website, click on the comment button below.
